Bandwagons. You’ve got to love them. But bandwagons are a dime a dozen. Every industry has one and far too many people end up getting hurt when they try to jump on them.
The health industry is no different.
The problem with bandwagons is that they tend to offer overly simplistic solutions to a complex problem. Vitamin D is a recent example of a health industry bandwagon. Every week there is a new study demonstrating the importance of Vitamin D in everything from depression to diabetes to cancer. And supposedly supplementing with Vitamin D will fix all of this. Maybe it will, but I doubt it. Answers are usually a little more complex than that.
The adrenal glands could also be considered a bandwagon of sorts because practitioners quickly assume they’re the cause of virtually every disease imaginable. But is focusing on the adrenal glands a legitimate approach when pursuing health, or a crude explanation for a much more complicated issue? Well… yes and yes.
A primer on the adrenal glands
The adrenal glands are small, triangular shaped glands that sit atop your kidneys, hence their other name “suprarenal glands” (from the Latin supra, or “above”). The adrenal glands regulate our body’s response to stress in a number of ways.
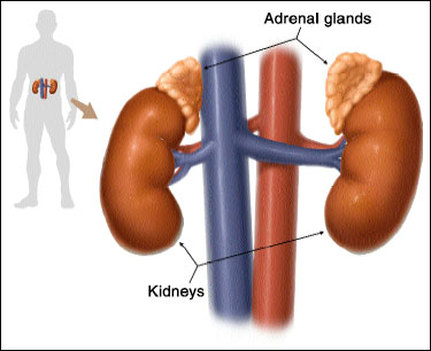
There are two main sections of the adrenal glands: the outer adrenal cortex and the inner adrenal medulla.
The adrenal cortex is further divided into three layers.
- Zona glomerulosa – the site of mineralcorticoid production (i.e. aldosterone), which helps to regulate sodium/potassium balance in the body
- Zona fasciculata – the site of glucocorticoid production (i.e. cortisol), which helps regulate blood sugar balance
- Zona reticularis – the site of sex hormone production (i.e. DHEA, androstenedione)
(In medical school, one way we learned to remember these three layers is: “Salt, sugar, sex… the deeper it goes, the sweeter it gets.” Not important, but catchy.)
The adrenal glands are unique in that part of them, the inner adrenal medulla, has a direct connection to the brain. In virtually all of the other hormone producing glands in the body, the message to secrete a hormone is transmitted via a chemical messenger traveling through the blood stream. For example, TSH, a hormone, tells the thyroid to produce thyroid hormone. ACTH, a hormone, tells the adrenal cortex to secrete cortisol.
Not so with the adrenal medulla. There is a nerve that goes directly from the brain to the adrenal glands. It’s like Commissioner Gordon’s red telephone to Batman. This makes sense. When you are in an acute stress situation (perhaps when the Penguin escapes), you want your body to respond quickly.
Adrenal glands gone awry
For simplicity’s sake, let’s break down adrenal function into two categories:
- Overactive
- Underactive
Overactive adrenal glands usually produce too much cortisol and possibly other adrenal hormones (i.e. epinephrine, aldosterone). Since cortisol plays a role in elevating blood sugar, this is often accompanied by an increased blood sugar level. Over time, this might end up leading to conditions like insulin resistance and metabolic syndrome.
Underactive adrenal glands, on the other hand, produce inadequate amounts of hormones, especially cortisol, to maintain homeostasis in the body. A common clinical problem with underactive adrenal glands is hypoglycemic symptoms due to fluctuations in blood sugar. Normal, healthy bodies release cortisol to help liberate glucose to maintain the functions of our brain, organs and cells when blood sugar levels decline between meals, or overnight during sleep. When cortisol is unavailable, glucose levels get too low. The adrenal glands release epinephrine (aka adrenaline) as their back-up plan. This causes the lightheadedness, shakiness and irritability that people with low blood sugar experience, and is why people with low blood sugar commonly wake up during the night.
What can cause dysfunctional adrenal glands? Unfortunately, a lot of things: mental/emotional stress, food sensitivities, blood sugar imbalances, infections (i.e. parasitic, bacterial), excessive exercise… basically anything that is a perceived stress on the body.
Adrenal physiology in the 21st century
Forty years ago, medical practitioners thought that the adrenal glands went through stages starting with overactivity (alarm phase), to a declining phase (resistance phase) and finally to underactivity (exhaustion phase).
This is a logical model, but it doesn’t hold up to current research. We now know that under the influence of certain biochemical processes, the adrenal glands can go straight into a state of overactivity or underactivity without going through the first two phases.
For instance, through a series of biochemical processes a viral infection can throw the adrenal glands into a state of adrenal underactivity. On the other hand, food sensitivities seem to encourage the body’s physiology to promote a state of adrenal hyperactivity.
Testing adrenal gland function
TRY THIS AT HOME!
Here’s one relatively easy test to do if you have a blood pressure monitor. It’s called the orthostatic hypotension test. After lying down for approximately 5 minutes, take your blood pressure and make note of the systolic pressure (the top number). Then stand up and take your blood pressure again.
If your systolic pressure remained the same or if it decreased, there is a chance you do not have optimal adrenal medulla function, or epinephrine secretion. When we stand, epinephrine is normally secreted to increase our blood pressure to help prevent gravity from pulling blood away from our brain. If your blood pressure drops, it might mean that epinephrine isn’t there to do its job.
| SYSTOLIC CHANGE | POSSIBLE FINDING |
|---|---|
| Increases 6-10 mm/Hg | Healthy adrenal function |
| Does not change | Fair adrenal function |
| Drops 1-10 mm/Hg | Poor adrenal function |
| Drops more than 10 mm/Hg | Adrenal exhaustion |
Another at-home test you can do is called the paradoxical pupillary reflex. Standing in front of a mirror in a dark room, take a flashlight and shine the light into one eye at a 45 degree angle from the side. Watch your pupil.
When in the dark, your pupil should be dilated (open). When you shine the light it should constrict. The duration of constriction can indicate adrenal function, though there are other causes for a positive finding on this test. Wait 30 seconds in the dark before repeating with the other eye.
| PUPIL CONSTRICTION | POSSIBLE FINDING |
|---|---|
| Stays constricted for at least 20 seconds | Healthy adrenal function |
| Fasciculates (pulses) after 10 seconds | Fair adrenal function |
| Fasciculates (pulses) in 5-10 seconds | Poor adrenal function |
| Immediate pulsation and dilation | Adrenal exhaustion |
LABORATORY TESTING
There are a few ways of assessing adrenal gland function using laboratory testing. By far the most popular is the adrenal salivary test. It takes four salivary samples throughout the day and uses them to assess levels of salivary cortisol and DHEA. Along with patient history, symptomaology, and clinical observation, the adrenal salivary test is one of the most effective ways of assessing adrenal gland function and determining a course of treatment.
As an aside… before you use hormone replacement
In practice and even on the Precision Nutrition Forum, people often ask about the use of hormone replacement. There are three things that must be functioning properly before consideration of HRT:
- adrenal gland function
- blood sugar balance; and
- gastrointestinal function.
Managing the adrenal glands
If you’re concerned about your adrenal glands, the first thing you must to is remove or address the source of stress. This may mean removing food sensitivities, addressing an infection, resolving mental/emotional stress, or whatever it may be that is negatively impacting adrenal gland physiology.
Once you address the source of stress, these are some therapeutic options depending on the findings of the adrenal salivary test:
- Adaptogenic herbs – There are a number of botanicals called “adaptogens” because of their amazing ability to help the body respond to stress. They can help dampen the stress response in overactive adrenal glands, and increase the response in underactive adrenal glands.
- Licorice root – This herb is used primarily in the case of underactive adrenal glands and can help with increasing circulating cortisol levels until the adrenal glands restore function. Due to its effects on aldosterone, it is not recommended for people with high blood pressure, though I think it can be safely used when monitored by a qualified medical professional.
- Phosphytidylserine – This compound is best known for its ability to lower cortisol. But its effects are understated. PS should be used in both overactive adrenal glands and underactive adrenal glands because of its profound effects on the hypothalamus, which is a key regulator in the feedback loop between the pituitary and adrenal glands. Though 600-800 mg taken orally seems to be effective, I personally like using a topical application of PS to get even higher doses while keeping costs down.
- Hormones – Even though I mildly bashed the use of hormone replacement, there are two hormones that are sometimes indicated when rehabilitating the adrenal glands: pregnenolone and DHEA. However, please don’t use them without the supervision of a qualified medical professional.
Summary
The adrenal glands and their hormones have major physiological impacts on our body including bone metabolism, hormonal balance, gastrointestinal function, thyroid function, brain health, blood sugar balance, inflammation, immune system function, etc. But in today’s modern times, supporting one’s adrenal glands is far more complicated than in the past. It requires proper testing, looking at many different physiological systems in the body, and proper nutritional support to help our body deal with stress. Unfortunately conventional medical doctors know nothing about this and many alternative doctors are using adrenal gland models that have become outdated.
About the author
Dr. Bryan P. Walsh is a Naturopathic Physician specializing in nutritional biochemistry, functional laboratory testing and natural medicine. He is a guest lecturer at the University of Maryland School of Medicine, has been a presenter at national conferences, and is currently an advisor to the Precision Nutrition team.
Comments:
Stress is a major part of life today. In the past stress was often matched with activity. For instance, getting chased about by a wild animal or excitement from having to catch something that has bolted away. Part of resolving stress could be to match the activity with the stress whenever possible to tackle problems with excess cortisol production.
Adequate rest is also essential. Most people are sleep deprived - trying to function on a few hours sleep most days. This is very stressful to the body. For a time the body can cope by pumping out large amounts of hormones to keep you functioning but over time glands (especially the adrenal ones) can become exhausted.
With prolonged pushing of the body to keep on doing what it is not meant to do certain systems break down and become less efficient at producing hormones at super optimal levels.
With inadequate supply of adrenal hormones diet is always something we can improve. Adding nutrients back in such as the fat soluble vitamin D analogues can help (there are many different natural forms of vitamin D in nature that are not supplied with artificial vitamin D supplements).
Some fat loss supplements cause adrenaline to be released to accelerate fat burning but constant stimulation causes exhaustion much more quickly than just a stressful life. Once you try to stop taking the supplements you can experience unusual lows in energy, prompting you to take the supplement again. If you are still inclined to take supplement that cause adrenaline to be released then do it cyclically (eg 1 day use followed by 3 days without). Also, do exercise after supplementation to take advantage of the large release in energy.
No comments:
Post a Comment